Community-led health and health inequalities -
frequently asked questions
Community-led health is a way for people in a community to take joint action to improve things for their community, leading to improved health and wellbeing.
This set of FAQs help to explain what community-led health is, and the context within which it works, in a simple and accessible way for people who are new to the issues or who simply need a refresher.
What do we mean (and not mean) by community-led health?
A community-led approach to health follows the social model of health which recognises that health and wellbeing is about much more than the treatment of disease and illness. This model links our health and wellbeing to the world around us, including our work, education, housing, leisure and to the way we organise ourselves as a society.
The community-led health approach supports communities experiencing disadvantage and poor health outcomes to:
identify and define what is important to them about their health
identify the factors that impact on wellbeing
take the lead in identifying and implementing solutions
Community-led health is not about the treatment of disease or health conditions by NHS medical services or interventions such as GPs, health clinics or hospitals.
Instead, community-led health puts the focus on communities as the mechanism for change, rather than the community as simply a setting for health practice.
This makes it fundamentally different than community-based health services, and different from the participation of communities in pre-determined health initiatives.
Ideally these different approaches should all work together, with community-led health being viewed as an important aspect of overall health and wellbeing policy. It can also help drive preventative approaches that focus on building and sustaining good health and to prevent ill health from occurring.
The social determinants of health: what are the factors which affect people’s health?
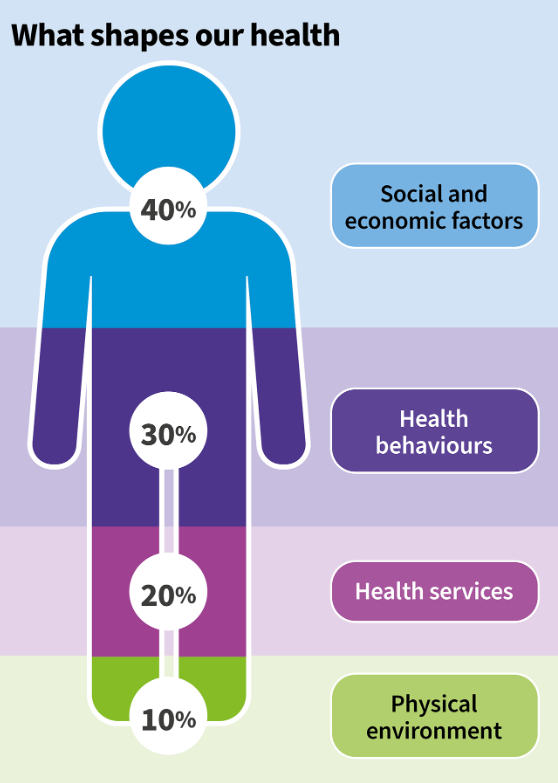
Social and economic factors, our physical environment and the ability of our health services to respond all contribute greatly to our health.
These factors greatly influence people’s health, far more than any individual lifestyle choices such as alcohol consumption, diet, smoking or any other factor that people can control. In addition to this, these individual health behaviours themselves are also shaped by the places and environments in which we live.
People living in poorer communities can be subject to a ‘double effect’: already living in overall worse social, economic and environmental conditions, they can face challenges and barriers when making individual health choices too – for example food insecurity or lack of outdoor space for walking.
These external social, economic and environmental factors and their impacts, both on health and health behaviours, are collectively referred to as the social determinants of health.
How do the social determinants of health affect health inequalities?
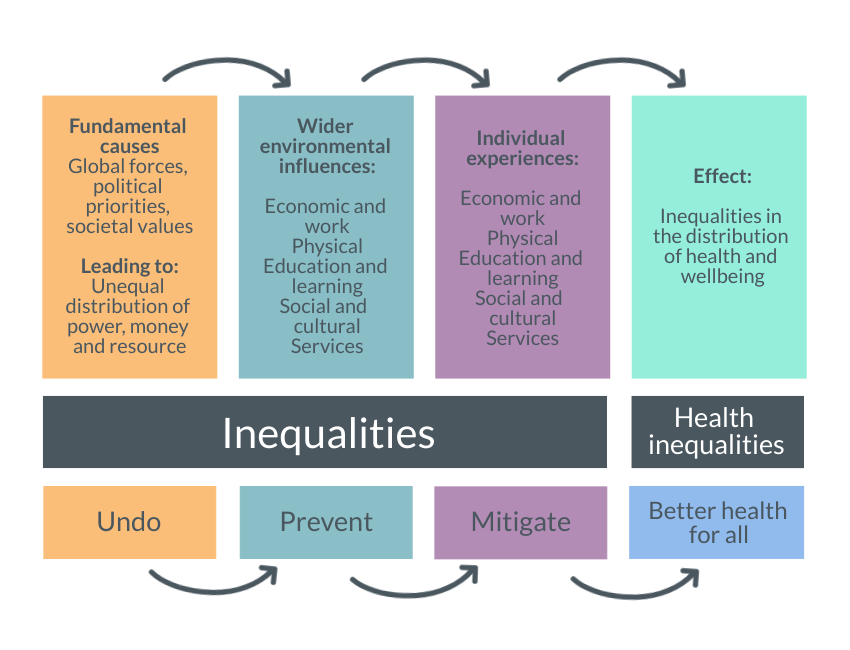
The social determinants of health are all the non-medical factors that influence health outcomes. They are the conditions in which people are born, grow, work, live, and age, and the wider set of forces and systems shaping the conditions of daily life. These forces and systems include economic policies and systems, social and cultural factors, environmental effects and political systems.
Because these factors affect every single area of life, they are different for everyone and every community. Existing widespread inequalities in areas such as income, housing, and physical environment then interact together to produce health inequalities.
For example, someone living in housing with a mould problem is more likely to develop lung problems, or someone who lives in poverty may have poorer health due to not being able to afford to eat regular, healthy meals. And these factors can all interact together to produce the widening health inequalities we see between our poorest and our more affluent communities.
This model describes the ways in which the determinants interact at the macro to micro level with inequality as the consequence.
How can we measure and track health inequalities?
There are two key measures we use when we talk about health inequalities: life expectancy (a measure of how long we can expect to live) and healthy life expectancy (how many of those years are expected to be in good health).
Provisional statistics on life expectancy published by National Records of Scotland (NRS) showed that in 2020-2022 the average life expectancy was estimated to be 76.5 years for males and 80.7 years for females.
However, those figures are simply the average across the country and do not show the concerning differences within the data.
In the most-disadvantaged ten percent of Scotland, men have a life expectancy of 68.6. In the least-disadvantaged, male life expectancy is 82.3 – a gap of 13.7 years of life.
For women, life expectancy in the most disadvantaged ten percent of neighbourhoods in Scotland is 75.0, but for the least disadvantaged it is 85.5 – a gap of nearly a decade.
The data on healthy life expectancy shows an even more pronounced inequality, with the healthy life expectancy gap of 26 years for men and 25 years for women.
The statistics above show how significant, unfair and unjust the effect of health inequalities can be. Widespread, worsening health inequalities in Scotland are causing people in our most deprived communities to effectively lose years of their potential lifespan and decades of good health, compared to those in our most affluent communities.
How does community-led health work in practice to tackle health inequalities?
Tackling inequalities is at the heart of how we improve Scotland’s health and make a fairer, healthier future for everyone.
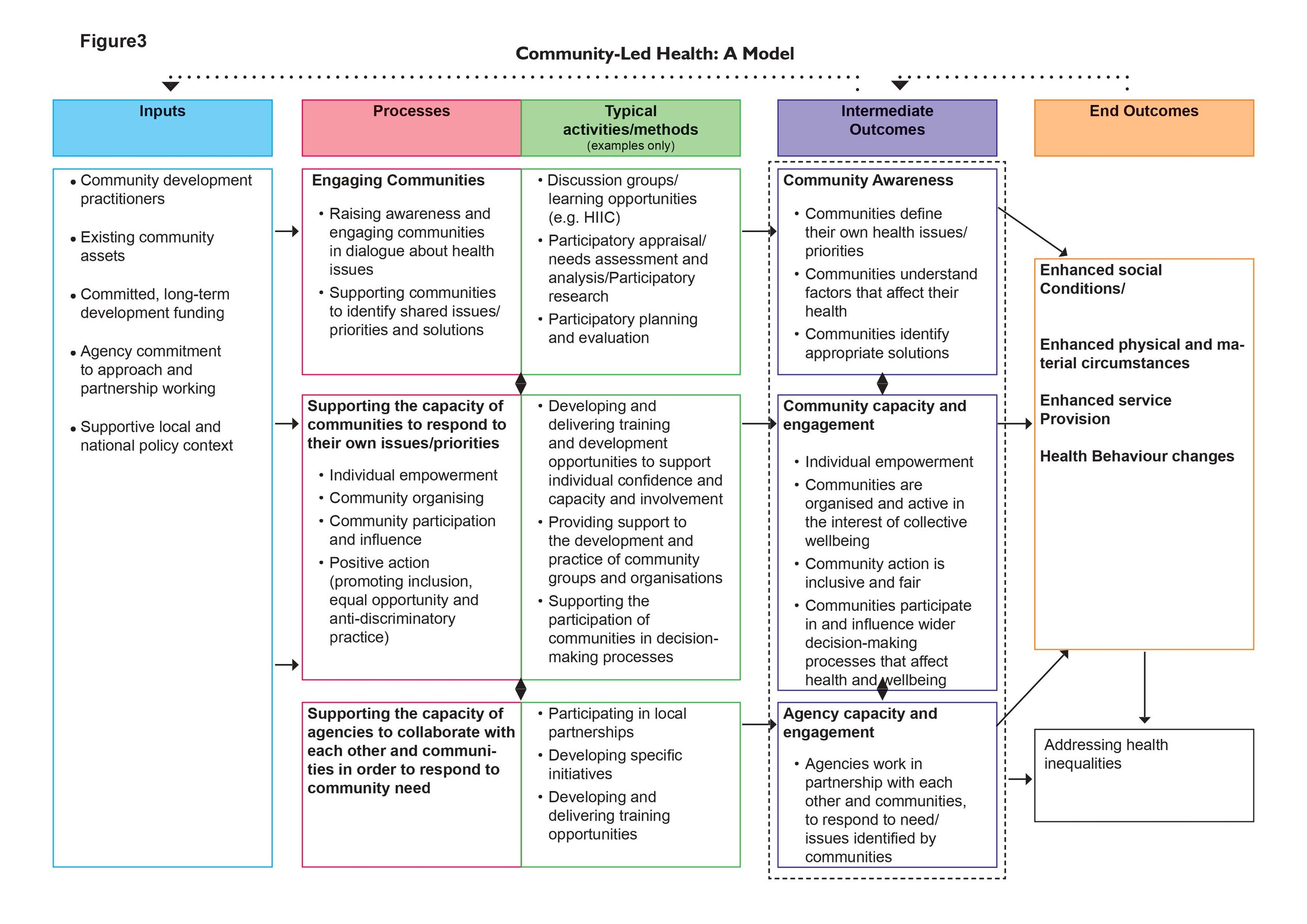
Community-led health can have a huge impact by targeting the provision of support to people and communities experiencing inequalities, disadvantage and marginalisation to take collective action, at both individual and community levels.
By helping communities to organise, community-led health creates opportunities for people and groups to actively address the wider causes of inequalities, not only in their local area, but also at a strategic level where community organisations engage in decision-making processes.
This is the recognised model for community-led health in Scotland (source). You’ll notice that the intermediate outcomes focus on individual and community empowerment, and the end outcomes are reflective of both improved health and physical and material circumstances.
It’s the targeting of this approach to specific groups and communities that directly impacts on inequalities, but also the collective gain for others when tackling wider issues affecting health.
Here are the types of things people working in community-led health do. You can see it is a long-term approach, embedded within communities and based on collective and collaborative action to support, facilitate and work to build sustainable change, driven by people themselves.
What actions do we need to take to ensure community-led health can effectively work to tackle health inequalities?
Our recent briefing paper outlines four key actions we can take to ensure that community-led health is able to effectively play its part in tackling Scotland’s widespread and worsening health inequalities. You can read much more about this and explore the four actions: Health inequalities in Scotland – Meeting Our Shared Challenge.